Knee Replacement Surgery
Total / Unicompartmental Knee Replacement
Surgery
You will be asked to come to hospital on the evening or morning prior to your surgery. On arrival you will have your blood pressure, pulse, oxygen saturation level and temperature measured. You will be sized for special stockings (TEDS) which are worn to reduce the risks of blood clots in your legs.
The anaesthetist and a member of the surgical team will visit you. They will discuss the proposed anaesthetic and surgery with you again. You will have the opportunity to ask any further questions. You will be asked to sign a consent form for the proposed operation once you are ready and all your questions have been answered.
Surgery usually takes 1 ½ to 2 hours. You will then be taken to the recovery room, where you will be monitored for about one hour. You will then be taken to your room on the ward.
When you awaken you will find you leg is firmly wrapped and you may have a small drain. The drain is to remove any bleeding from the knee; it usually comes out after 24-48hrs on the ward. A drip will be in your arm. The drip makes up for the lost fluid, which may have occurred in your operation and is used to dispense blood or drugs that you may require. The drip is usually removed 48 hours after surgery. You will be given regular pain relief by the nursing staff in the form of an injection or tablet as required. (See section on pain relief following surgery) You may also have a urinary catheter which will remain until you are more mobile.
The recovery from the operation requires about 4-5 days in hospital for a TKR and 2-3 days for a UKR. In this time, usually the day after surgery you will commence your rehabilitation with physiotherapy. This involves exercises to improve the strength of the muscles and to regain the range of motion of the knee. On the day after surgery your physiotherapist will begin to assist you to get out of bed and walk a small distance. This will be progressed over the next few days, until you are independently mobile.
The exercising and mobilising of the knee will cause some discomfort and swelling, this is normal, and is just part of the healing process. Any swelling and discomfort in the calf muscle should be brought to the attention of the nursing staff as you may require further investigations for this.
Potential Complications and how to reduce them
Despite the success of total joint replacement, there is a small risk of developing complications. These complications can develop because of health problems, the anaesthesia or the surgical procedure itself.
Possible local complications include: surgical site infection, damage to blood vessels and nerves, blood loss possibly requiring blood transfusion, bone or implant fracture, increased bone formation around the joint, dislocation of the joint, altered limb length, early wear of the prosthesis, and persistent or worsened pain and stiffness in the joint that was replaced. These complications may require additional surgery to improve your function.
Other medical complications include the risk of developing a deep venous thrombosis, pulmonary embolism, heart attack, stroke and even death. Although the likelihood of such complications occurring is low, your surgical team will make every effort to minimize the risk as much as possible. Your surgeon, anaesthetist and medical team will discuss these issues with you before surgery. Please make sure all your questions are addressed when you meet with your surgical team.
Infection is a possible complication of any surgery. The risk is reduced through careful surgical technique and the use of antibiotics before your surgery. Bacteria can travel through your bloodstream from infection elsewhere in your body to your new joint, i.e. from your throat, teeth, skin or urine. This is why it is important to have all infections assessed and treated before your surgery, as well as after surgery to protect your new joint. Antibiotics are administered intravenously at the time of your surgery. (Any allergy to any known antibiotics should be brought to the attention of your surgeon or anaesthetist). Despite these measures, there is still a chance of developing an infection but this is less than 2%. Normally these are superficial wound infections that resolve with a course of antibiotics. Occasionally serious infections occur that require further hospitalisation and treatment. Sometimes they necessitate removal of the knee replacement for a period of time; antibiotics are administered via a drip for a few weeks, prior to re-implantation of another knee replacement.
Breathing Problems such as pneumonia can occur after surgery. It is important to do several deep-breathing and coughing exercises every half hour when awake the first few days after surgery. This helps provide oxygen to your lungs and keeps your airways clear. Sitting up, getting out of bed as soon as possible and being active also helps prevent breathing problems.
Cardiovascular Complications (heart problems) can occur due to the stress of surgery. Surgery puts an additional workload on the heart. In patients with known heart disease, this can increase the risk for abnormal heart beats, chest pain or very rarely, heart attack. These complications can also happen in patients with no known heart problems. This is why it is important to have a thorough health assessment before your surgery.
Deep Vein Thrombosis (DVT) are blood clots which can develop in the deep veins of your legs. This is often associated with lack of movement, so getting out of bed and being active as early as possible is encouraged. It is important to move your ankles up and down several times an hour after surgery. This is called “ankle pumping”. You should also tighten and release the muscles in your legs. These exercises promote good circulation. Anticoagulants (blood thinners) will also be used to prevent blood clots. They are given in either a pill or needle form. A combination of immobilisation of the limb, smoking and the oral contraceptive pill or hormonal replacement therapy all multiply to increase the risk of a blood clot. Any past history of blood clots should be brought to the attention of the surgeon prior to your operation. The oral contraceptive pill, hormonal replacement therapy and smoking should cease 6 weeks prior to surgery to minimise the risk.
Pulmonary Embolism can occur when blood clots from the deep veins in the legs or pelvis break off, travel up to the lung and lodge there. If the clot is large enough, blood circulation to the lungs may be cut off. This is a serious complication. Anticoagulants (blood thinners) are given after surgery to prevent clot formation. Ankle pumping and early activity will also help prevent this complication.
Urinary Problems, such as difficulty passing urine, can happen following any type of surgery. Sometimes a catheter (soft plastic tube) is placed in the bladder to drain urine. The catheter can be left in place for a few days or removed immediately after the bladder has been emptied. Let your nurse know if you have problems passing urine. Following spinal anaesthesia you may pass some urine without being aware of it. This is normal and can happen during the first few hours until the spinal anaesthesia wears off.
Nausea is common after surgery. Medication may be given to settle your stomach, so let your nurse know if you are experiencing this. In order to minimize nausea, it is important to take your pain pills with food to protect your stomach.
Paralytic Ileus is a distention of the bowel with gas. This can happen when the bowels stop working properly. As a result, gas builds up and causes abdominal discomfort, bloating and vomiting. To prevent this, early activity is important to stimulate your bowels to function normally.
Constipation can occur because pain medication can make your bowels sluggish. Stool softeners are given twice a day to help prevent this. If they are not effective, ask your nurse for a laxative. Make sure your bowels have moved the day before surgery to help prevent problems after surgery. Lots of fluid, a high fibre diet and activity also help.
Allergic reactions can happen after surgery and vary from a mild rash to an intense reaction that can interfere with your breathing. Please let us know if you have any allergies. They will be documented in your medical record. We will also provide you with an allergy alert bracelet to be worn while you are here.
Skin Irritation and bed sores are caused by pressure from lying in bed. It is important to change your position frequently while in bed and to get up as much as possible after surgery. The nurses and therapists will help you.
Confusion and Delirium can sometimes occur in older people after surgery. You may behave differently, and see or hear things that aren't really there. This usually resolves in a few days, but can last for several weeks. Many things can contribute to this, such as the anaesthetic, pain medication, lack of sleep, and alcohol withdrawal. It is important to let us know if you have experienced this with previous surgeries. Wearing your glasses and hearing aids can help if you experience this. We also recommend that you reduce your alcohol intake several weeks before your surgery. If you have experienced postoperative confusion in the past, it is helpful to have a relative sit with you after surgery.
Stiffness, sometimes the knee becomes stiff after surgery (1%) due to scar tissue forming inside the knee. If this happens the knee may require a manipulation under a second general anaesthetic to help regain movement.
Pain following a TKR/UKR: A small number of people after knee replacement surgery continue to experience some pain. Sometimes no obvious mechanical cause for the pain can be found. Research and studies done have shown that 10 – 15% of patients still have some ongoing pain and are not fully satisfied after their surgery. There isn't any specific reason to explain why this is the case but majority of this sub group of patients still feel that this post-operative pain is still better than their previous arthritic pain and doesn't impede on their function. An important point to note is that overall recovery and improvement following a Total Knee Replacement can sometimes take up to 2 years.
If you are in this group, you will be investigated further to rule out any significant causes for this pain. Treatment for this involves medical management of the pain, and specialist rehabilitation.
Excessive Bleeding: Inevitably some blood is lost at the time of surgery. Sometimes people lose larger volumes of blood and a transfusion may be required. Bleeding is more likely to occur with patients taking aspirin or other anti-inflammatory drugs. They should be stopped at least one week prior to surgery.
Tendon, nerve or blood vessel damage: Very rarely these structures can be injured during the operation. Normally they recover, but occasionally patients may experience extensive bruising or have difficulty moving their foot up and down. Often after a knee replacement patients have a small patch of numbness to the outside of the scar due to small nerves in the skin being damaged; this normally does not cause problems and often diminishes with time.
Aseptic loosening requiring Revision surgery Over time the components of the knee replacement can wear out or become loose. This normally presents with worsening pain and may require further surgery to put a new knee in. On average, about 85-90% of the TKRs will last 14-15 years and about 85-90% of the UKRs will last 9-10 years.
Dislocation of the bearing (specific to UKR) The UKR has a mobile plastic bearing. Rarely this can dislocate and require further surgery to reposition it (<1%).
Remember: Getting out of bed and walking as soon as you are able will help prevent many of these complications and allow for a smooth recovery.
After Your Knee Replacement
Rehabilitation and Knee exercises after surgery
The following information has been designed to enable you to start your rehabilitation in hospital and continue at home. Your physiotherapist will work through this information with you prior to discharge and will be happy to answer any queries.
Phase 1. Day of operation (Day 0) to Day 3
The exercises are the same whether you have undergone a UKR or TKR. If you have had a UKR you may be able to progress more quickly.
- Ankle pumps: Move your feet up and down regularly to help the blood circulation in your legs
- Static Quadriceps contraction: Sit or lie with your legs stretched out in front of you. Tense your muscles on the front of the thigh by pushing the back of your knee down into the bed and pull your toes toward you. Hold for a count of 5 seconds. Relax completely then repeat.
- Inner Range Quadriceps: Sit or lie on the floor or a bed, place a firm cylinder wrapped in a towel under your knee. Push the back of your knee down into the towel and straighten the knee. Hold for a count of 3 seconds, as you get stronger increase hold up to 10 seconds. Relax completely then repeat.
- Knee bending exercise in lying: Sit or lie with your legs stretched out in front of you. Slide your heel up towards your bottom, allowing your knee to bend. Slide your heel back down again. Relax completely the repeat.
- Knee bending and straightening in sitting: Sit on a sturdy surface with your feet on the floor. Straighten the knee as far as you can aiming to get the knee completely straight, hold for 3 seconds then slowly lower your leg. Then bend your knee back as far as possible, by sliding your foot along the floor. Relax and then repeat
Phase 2: Exercises from Day 3 onwards.
This may be a few days later if you have had a TKR (day 6 onwards). Continue exercise 1-5. But add in following exercises.
- Knee bending exercise in standing: Stand with hands supported on a table or high backed chair, bend you knee by taking your heel towards your bottom and count for 5. Lower heel back to ground, relax completely and then repeat.
- Sitting to standing: Sit on a firm chair with arm rests. Bend both of your knees as far back as possible keeping your feet flat on the floor. Stand up fully and then sit down. Repeat.
- Step up and down: Stand at the bottom of a flight of stairs and hold the banister for support. Place foot of operated leg onto the first step. Hold for a count of 3-5 seconds then step down. Repeat.
Returning to Work
Most patients do not return to work until at least 6-8 weeks after their knee has been replaced. However, some patients return to work earlier if their job is sedentary in nature. When returning to work, be sure your daily work schedule allows time for your exercises. Make sure you start off with lighter duties and gradually build your way up to your regular work activities. Talk to a member of our health care team if you have specific questions regarding returning to work after your surgery
Community activities
Resumption of Driving
Driving may be resumed after 6 weeks unless advised otherwise by your surgeon. Check with your insurance company about any concerns you may have regarding coverage when you resume driving.
Getting Into the Car or Van
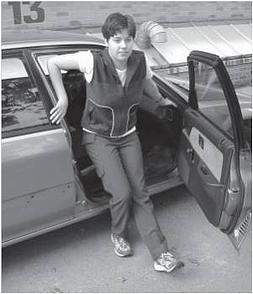
You will be able to sit in the front passenger seat of most vehicles. You will need to take rest breaks if you are travelling for long distances.
It is easier to get into a car if you and the car are on the same level (do not stand on a curb or be too close to the curb). Have the driver slide the passenger seat as far back as possible and recline the backrest. Back up to the car seat using your walking device until you feel the car against the back of your legs. Extend your operated leg(s) directly out in front of you. Sit down slowly holding onto two stable surfaces. These may be the dashboard and the frame of the car (avoid holding onto the car door). Using your arm strength, slide onto the seat so that both legs are supported on the car seat. Slide your legs in, one at a time. Once you are facing forward, the backrest of the seat may be raised back up.
Getting Out of the Car or Van
Recline the backrest. Shift towards the driver's side of the vehicle until you can slide your legs out one at a time. Slide to the edge of the car seat, extend your operated leg(s) out in front of you and push up off the car seat.
Resuming an active lifestyle
When you can begin doing your leisure activities following surgery depends on the physical demands of the activity and your stage of recovery. For more information please consult the exercise booklet provided to you by your physiotherapist during your hospital stay.
Activities That May be Resumed Immediately
- Walking
Walking is a fantastic exercise for your new knee replacement. Initially with short distances, but as the knee becomes more comfortable the distances can be increased. Points to aim for when walking:
- Step length. Make sure both steps are equal
- Timing. Try to spend the same length of time on each leg
- Always put the heel of each foot to the ground first
- Always put the heel of each foot to the ground first
Activities That May Be Resumed after 6 Weeks
- Swimming – You may be able to swim or do exercises in the pool if your incision is well healed and if you have access to a pool with a graded entry (stairs with hand railing) after the 6 week period. (Discuss this with the surgeon at you first post-operative check at 6 weeks)
- Driving
- Stationary biking
- Golf – begin at the driving range
- Gardening. It is recommended that patients use a “kneeling platform” that is padded and has handles to allow easy transition from kneeling to standing.
Activities That May Be Resumed at 3 Months
- Golf
- Outdoor cycling (NOT Mountain Biking)
- Doubles tennis
Activities to Discuss With Your Surgeon
- Skiing – downhill or cross-country
- Ice skating
- Sailing
- Canoeing
- Mountain biking
High Risk Activities that should be avoided
- Singles tennis
- Jogging / Running
- Squash / Racquetball
- High impact aerobics
Discharge Instructions and follow up
Visit your nearest Emergency Department if you have any of the following:
- Shortness of breath or difficulty breathing
- Chest pain, tightness or pressure
- A significant increase in pain, swelling or redness in your calf/ calves
- A sudden, unexpected, severe increase in pain in your new joint
Notify your surgeon / GP immediately if you have any of the following:
- Increased redness, swelling or a sudden increase in bruising around the incision site
- Drainage from the wound for more than 4 days after discharge
- A foul odour or yellow or green drainage at the incision site
- Excessive bleeding
- Any other signs or symptoms of infection (i.e. bladder infection, tooth infection, etc.)
- A persistent increase in your temperature (over 38ºC)
Kneeling
Patients often feel uncomfortable kneeling after a TKR/ UKR. This may be due to pressure on the wound and some numbness around the scar. The new knee will not come to harm if you kneel on it. It is wise to check the ground carefully before kneeling as if you have some numb patches of skin you may kneel on sharp objects without realising it.
Bathing and showering
It is best to avoid getting your wound wet until it is dry and the stitches clips have been removed (normally about 10 – 14 days after the operation). Once the wound is dry you may bath and shower as normal. Take care getting in and out of the bath or shower unit with wet and slippery surfaces, as your knee muscles will not yet have regained full strength.
Looking after your wound
As your wound is healing it often feels hard and itchy, this is normal and settles with time. You may find the skin is numb on one side of the wound; this normally improves with time but may not come back to full normality. It tends not to cause any long term problems. Avoid contact with the wound, it is best to leave it covered up with dressing until the clips and sutures are removed (around 10 – 14 days).
If you notice the wound is discharging/ leaking it is best to seek medical advice, you should ring your GP or the surgical team.
Pain control
Having some pain after your operation is normal. Keep in mind that each person feels pain differently. What is moderately or very painful to some may be mildly painful to others. Pain can be relieved by:
- Balancing rest and activity
- Using ice to help reduce pain and swelling – use it for 10 minutes at a time for maximum benefit
- Elevating your leg above your heart level to help reduce swelling, pressure and pain
- Take pain medication as ordered. Avoid alcoholic beverages while taking pain medication.
- When you are ready, talk to your GP or pharmacist about how to reduce your use of medication.
- If your pain is not well controlled, call your GP
- Common side effects of pain medicine are constipation, nausea or vomiting, and sleepiness.
- CONSTIPATION: If you experience constipation, you should increase your fluid intake, eat foods that are high in fibre and increase your activity. Drinking prune juice may help. You may also need a laxative, such as senokot, to get your bowels to move.
- STOMACH UPSET: If you experience nausea, take your pain medicine with food. You can also take medication to settle your stomach. Talk to your pharmacist or family doctor about what medication would be best for you.
- SLEEPINESS: If your pain medicine makes you sleepy you can try taking a smaller dose, for example, one tablet instead of two tablets.
Dental and other medical procedures
It is important to let your dentist and other health care providers know that you have had a joint replacement. Antibiotics should be prescribed before dental work or other surgical procedures to prevent bacteria from infecting your new joint.
Contact your dentist or doctor a few days before any procedure to ensure that you are given a prescription.
Sunnybrook's Holland Orthopaedic & Arthritic Centre has developed part of this material and this has been edited by Mr. Fahad G. Attar. Permission to add this link to our website has been granted by Sunnybrook Health Sciences Centre. Copyright 2012 by Sunnybrook Health Sciences Centre, Toronto, Ontario. All rights reserved.
